Currently chorionic villus sampling (CVS) and amniocentesis are the main methods for prenatal genetic diagnosis. Both these procedures are invasive and have been associated with a risk of pregnancy loss of 1% ; also, cells need to be cultured for the obtainment of a karyotype, and two weeks are commonly required before the results can be made available to the pregnant woman. A further problem with amniocentesis is that the technique is performed at 16–18 weeks’ gestation, and this results in the late termination of affected pregnancies with a more traumatic method and an evident psychological distress.
Quantitative fluorescent polymerase chain reaction (QF-PCR) has recently entered the field of prenatal diagnosis to overcome the need to culture fetal cells, hence to allow rapid diagnosis of some selected chromosomal anomalies
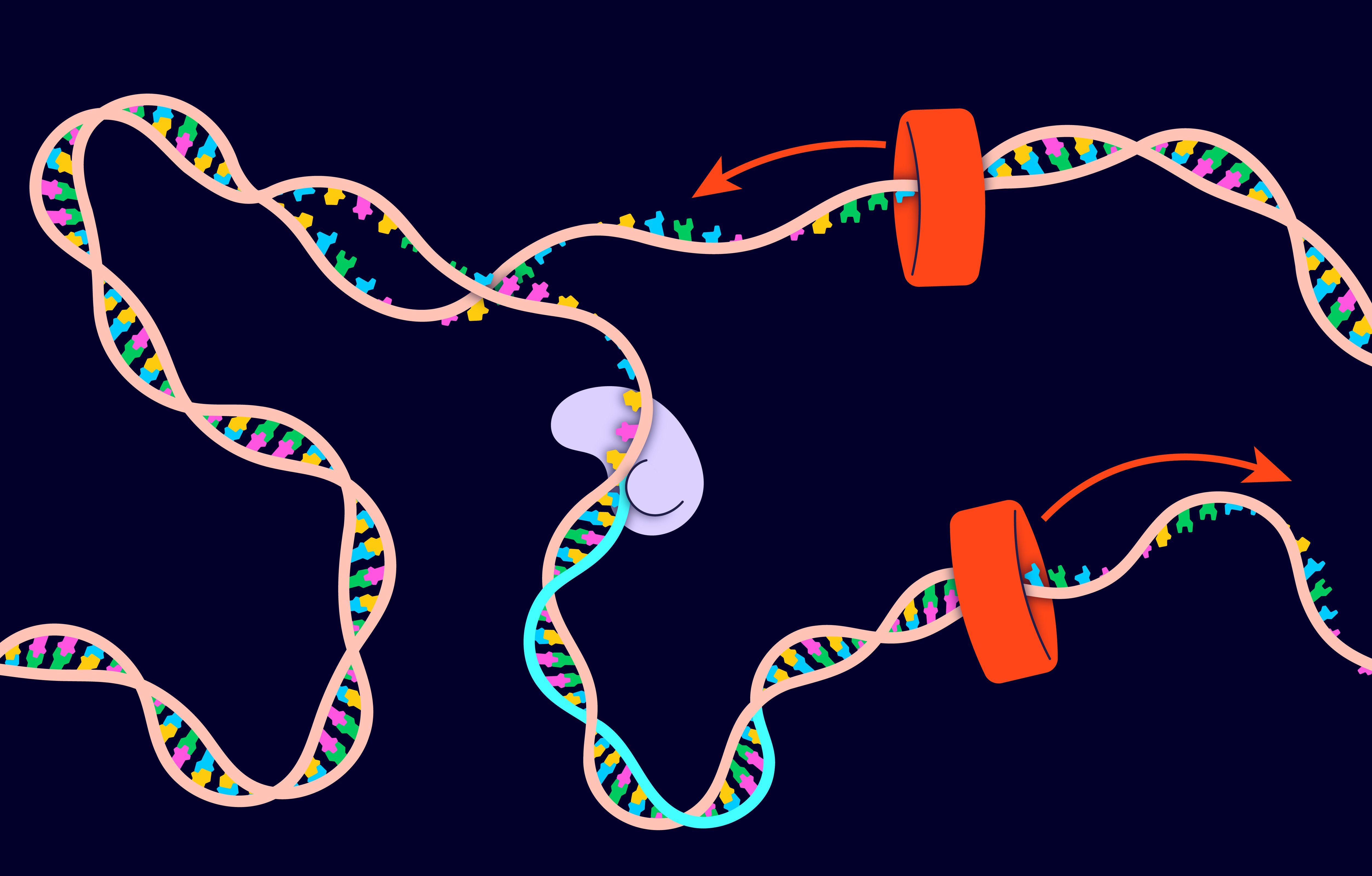
The QF-PCR technique relies on the amplification of chromosome-specific short tandem repeat (STR) sequences using fluorescent primers, whereas the analysis of the products of amplification is performed using an automated DNA sequencer. Usually STRs with high degree of polymorphism are used, and more than one STRs for each single autosomal chromosome are investigated at any one time in order to achieve informative results on the chromosome copy number; while the lack of highly polymorphic markers had hindered the detection of sex chromosome abnormalities until a few years ago, in recent times many of these markers have been identified, and the QF-PCR analysis of all numerical sex chromosome disorders has finally became possible
The detection rate of aneuploidies of the selected chromosomes (13, 18 and 21, and X and Y) was 98.6% (95% confidence interval 97.8–99.3).